It’s a bewildering sight. Athletes seemingly in peak physical condition collapsing without warning. Though rare, sudden cardiac death is still considered the leading medical cause of death among athletes — especially young adults.
Many times, the medical event can be traced back to hypertrophic cardiomyopathy (HCM), a genetic disease that causes the heart to contract more than it should. This leads to thicker than normal heart muscle, which impairs blood flow and makes it harder for the heart to pump blood. Affecting an estimated 1 in 500 people in the U.S., it’s the most inherited heart disease, according to the American Heart Association.
However, University of North Texas research could be key to developing more effective treatments for HCM in the future. It’s work that’s been more than a decade in the making for UNT biochemist Douglas Root, associate professor of biological sciences who specializes in the molecular structure of muscles and proteins.
“There is a drug on the market that can treat HCM, but it doesn’t really work well for young adults, so we still need more drugs along these lines,” Root says. “We hope our research can be a foundation to develop potential treatments that will be effective for more people with this disease.”
Root’s College of Science colleague Amie Lund examines an unseen foe for cardiovascular health — air pollution. In mechanical engineering, Hamid Sadat and his team developed a computational model to better understand how calcific aortic valve disease occurs. In biomedical engineering, Fateme Esmailie is using artificial intelligence and 3D-printed models to study cardiovascular fluid dynamics, and Huaxiao “Adam” Yang’s is creating organoids to advance a tissue engineering system for modeling and treating cardiovascular diseases.
Collectively, the research from UNT experts, funded by the U.S. National Institutes of Health, American Heart Association and others, is producing a much deeper understanding of the heart and could contribute to more effective treatments for heart diseases — the leading cause of death in the U.S. for more than 100 years.
A New Peptide
Hypertrophic cardiomyopathy happens when people have mutations in the genes that are responsible for heart muscle protein production.
“Those mutations make the protein structure less stable,” Root says. “So, this particular peptide that we’ve designed will bind to the protein myosin filament strands in heart muscle to hold them together and make them more stable,” says Root, whose research has been funded by the U.S. National Science Foundation and most recently by the NIH.
For his NIH-funded project investigating the new peptide to help with HCM, Root has worked with researchers at King’s College London, University of Kentucky, University of Missouri and Washington State University in Pullman.
“We designed the peptide at UNT, and our collaborators have helped us develop it further and test it,” says Root, who is the named inventor on a pending U.S. patent for the peptide.
Fundamental research for the novel peptide has been ongoing since 2011 at UNT. Alysha Joseph (’13) contributed to the work as a teenager in UNT’s Texas Academy of Mathematics and Science, which encourages its students to get involved in research at the university. It was her first experience with scientific research and inspired her current career journey.
“I had results that were somewhat positive and promising after my time in Dr. Root’s lab, but in my mind at that time, clinical translation seemed like a faraway dream,” says Joseph, who recently talked with Root about being named a co-author on a forthcoming paper including research she completed as a TAMS student.
Now a first-year cardiology fellow at UT Southwestern Medical Center, Joseph has continued her interest in HCM and the study of the heart. During her combined residency in internal medicine and pediatrics, she examined outcomes of patients who were born premature and how it affects their hearts as they get older.
“We know that hearts in people born prematurely tend to be smaller and stiffer,” Joseph says. “And over time, they can develop pulmonary hypertension and diastolic heart dysfunction. Knowing this population is at risk for these problems earlier in life, we could start screening them at a younger age to hopefully prevent these complications.”
Unseen Foe
Amie Lund, UNT associate professor of environmental toxicology, is hoping her research can help prevent heart problems for people down the road as well. She has conducted research related to the heart for more than 20 years — supported by millions of dollars in grants from the NIH and the U.S. Environmental Protection Agency.
“The heart is often thought of as just a pump, but its proper function is critical to life, providing the oxygen and nutrients that our cells need to survive,” says Lund, who is director of UNT’s Advanced Environmental Research Institute, which unites researchers across disciplines for projects focused on mitigating environmental problems in the world.
“The heart is often thought of as just a pump, but its proper function is critical to life, providing the oxygen and nutrients that our cells need to survive."
-Amie Lund, associate professor of environmental toxicology
It’s well documented that genetics, diet and lifestyle can impact heart health, but Lund’s lab asks questions about how exposure to common environmental air pollutants can contribute to a range of health problems from obesity to cardiovascular disease.
“For the last 30 years, we’ve known that on days of high air pollution, we see a higher incidence of heart attacks and strokes,” Lund says. “We have the clinical data to back that up, but we still don’t fully understand what’s happening in blood vessels and in the heart that contributes to these conditions. And so, our research investigates how exposure to these air pollutants can lead to these outcomes in the body.”

In urban areas such as the North Texan region, a major culprit causing poor air quality is pollutants generated from vehicles on the road, she says. That’s why Lund and her team of researchers, such as Honors College biology student Kennedy Stevens, are examining how pollutants like car exhaust are altering signaling pathways in the body. Specifically, they’re looking at the renin-angiotensin system, which is responsible for regulating blood pressure.
“We’re trying to tease out which of these signaling pathways in our body could possibly be a target for a pharmaceutical prevention or therapy,” Lund says. “And more importantly, if we know which components coming out of our vehicle exhaust that are particularly harmful to our bodies, then there is evidence to advocate for policy change that could reduce human exposure to these pollutants.”
Stevens (pictured third from right) investigates whether exposure to exhaust can cause the production of inflammatory proteins in the heart, which indicate early development of cardiovascular disease.
“I really like the applications that biology can have to improve the health of people,” says Stevens, who wants to become a research scientist after graduation, possibly working in the pharmaceutical industry or for the government. “That’s what drove me to join Dr. Lund’s lab because the research we’re doing now could have real-life implications.”
Modeling Disease
A few miles from the main campus in Denton at UNT’s Discovery Park — the largest university research park in the North Texan region — Joel Aboagye also has focused on HCM in his research.
As a graduate student researcher in Huaxiao “Adam” Yang’s Cardiovascular Tissue Engineering Lab, Aboagye utilizes human-induced pluripotent stem cells to grow cardiomyocytes — muscle cells in the heart. It’s a tedious task that can take up to a month to complete, but once ready, Aboagye can use the cells to conduct an in vitro study of the toll HCM takes on the heart.
“I’m looking specifically at the mechanical aspect, so how cell interactions and external forces influence gene expression and disease progression,” says Aboagye, a Ph.D. student in biomedical engineering. “This disease has a complex pathology, and its progression is not fully understood, but hopefully our research can shed more light on how HCM manifests at the cellular level.”
In Aboagye’s native country of Ghana, the prevalence of heart disease is increasing, which is partly what’s driving him to dedicate his career to finding solutions for prevention and treatment. He’s especially interested in how new technologies like those being developed in regenerative medicine and tissue engineering can advance personalized therapies for cardiac disease.
They’re similar interests shared by his faculty mentor Yang, who is investing in a methodology he believes could revolutionize disease modeling and drug discovery research. Using human pluripotent stem cells, Yang can develop cardiac organoids — microscopic tissue that can mimic intricate heart functions and structures, enabling his team to study human heart physiology and diseases outside a living human.
Yang and his current and former students have five pending U.S. patents for tissue engineering research methods and tools they have developed. Last year, Yang’s team also was named one of 20 winners in an NIH challenge competition focused on identifying alternative research methodologies that could model human biology.
“Engineering can be complicated, but I want to perfect a cardiac tissue engineering system that’s simplified and easy for people to use,” says Yang, assistant professor of biomedical engineering.
In addition to the HCM project Aboagye is working on, Yang’s lab is tackling other research, including early heart defects in babies using the in vitro modeling and investigating a range of interventions to determine if any are viable candidates to assist in repairing damaged heart tissues. The lab is dabbling in AI as well to look at drug-induced cardiovascular toxicity caused by a widely used cancer drug. For that work, Yang is collaborating with his UNT colleague Yunhe Feng, assistant professor of computer science and engineering who focuses on how people can use AI technology responsibly and fairly.
“We have biweekly meetings and are giving our students a chance to experience both of our labs,” Yang says. “This allows our students the opportunity to communicate and collaborate with researchers from a discipline other than their own.”
Shape of the Heart
AI and machine learning are essential in the research of biomedical engineering assistant professor Fateme Esmailie, too. She studies adverse heart complications after surgery, specifically what conditions lead to blood clots following a transcatheter aortic valve replacement (TAVR).
“TAVR is a minimally invasive procedure that involves placing a new valve in the heart using a catheter. While TAVR is generally effective, 15 to 20% of patients develop a complication known as thrombosis (blood clot formation inside the body), which impairs valve function, raises blood pressure and increases the risk of strokes,” Esmailie says.
Using AI can cut down the time it takes to solve the mathematical equations needed to understand the fluid dynamics in the body for her work. For instance, she says it could take up to one or two weeks to solve fluid dynamics equations representing one heartbeat for a patient-specific heart model, but AI can be used to develop alternative methods to extract the required information in a few hours or less.
Esmailie has long been fascinated with how the heart works. In her postdoctoral fellowship at the Georgia Institute of Technology, she developed computational models to analyze patient data and determine factors that could lead to thrombosis following a valve replacement surgery.
“Based on our AI-driven analysis of patient data the blood velocity and the height of the coronary arteries are significant predictors of thrombosis risk following transcatheter aortic valve replacement. However, these findings are preliminary, and we cannot fully trust these results until we have a larger dataset to train and validate our model,” Esmailie says.
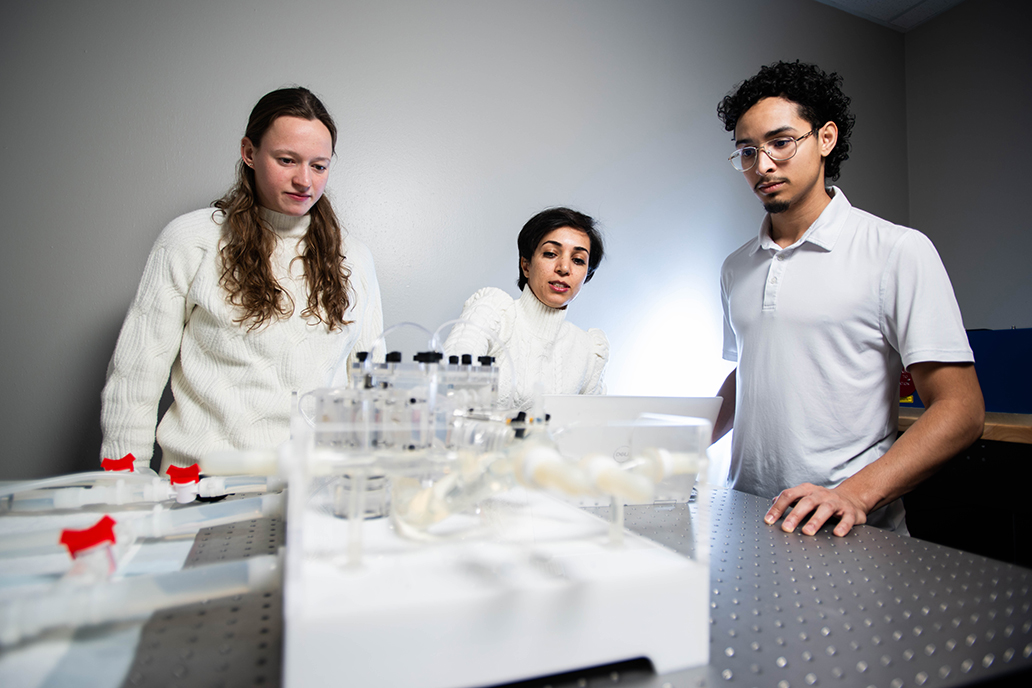
In her Thermal Fluid Assisted Medicine Lab, Esmailie has continued research along those lines with one of her current projects that recently earned funding from the American Heart Association. By using a combination of machine learning and experimental methods, Esmailie and her team are conducting further investigations on why blood clots happen after valve replacement surgery and what risk factors to look out for.
“Machine learning helps us cut down computational time, but we only have a limited amount of patient data to work with and this makes the AI-based model unreliable,” Esmailie says. “That’s where our 3D heart models come in. We can use those in vitro models to generate more data to better understand this condition.”
Master’s student Ricardo Rodriguez (’22) is one of Esmailie’s research assistants. When he first started in her lab, he was conducting computer simulations on blood flow. Now he’s responsible for creating the silicone-based 3D heart models that will be used in the experiments.
“I’m learning that human hearts vary from person to person, and that can impact whether you’re at risk for disease,” Rodriguez says. “So, what we’re looking at is how these geometric changes in the heart might contribute to the likelihood for heart complications.”
Complex Machine
Another variance in the body could be based on gender, as assistant professor of mechanical engineering Hamid Sadat has found. The aortic heart valve, for instance, is usually larger in men compared to women, making men more susceptible to calcific aortic valve disease — a condition in which calcium deposits build up on the aortic valve causing it to thicken and become stiffer. Once calcification happens, the valve can’t open and close completely, which impedes blood flow in the heart.
With funding from the NIH, Sadat has studied the condition for the last four years with collaborators from Baylor University Medical Center and Stanford University. They aim to learn more about how calcification happens to better diagnose and treat it. It’s presented a unique challenge from his other research, which uses fluid dynamics modeling and simulations to understand ship hydrodynamics for the U.S. Navy.
“I thought those Department of Defense projects would be the most challenging to deal with, but I realized the human body is super complicated,” Sadat says. “We had to develop more methodology and techniques to be able to study this aortic valve calcification.”
Sadat’s former doctoral student Kingora Kamau (’22 Ph.D.) and current doctoral student Mishal Raza-Taimuri created one such method — a computer model and numerical technique to better simulate blood flow in the heart. The UNT researchers feed the code for that model into supercomputers at the Texas Advanced Computing Center to solve the millions of mathematical equations needed to predict fluid dynamics and structural behavior of the heart.
The aortic valve is made up of three crescent-shaped sections or leaflets that help regulate blood flow. When calcified, these leaflets get stiff and have difficulty moving. Sadat says the UNT team modelled biotransport near the leaflets to understand the mechanism of calcification, the calcification patterns on each leaflet and how these patterns vary across different leaflets. So far, they found that calcification doesn’t appear uniformly across all three leaflets.
“It’s really interesting how complex these systems are in the body when compared to the best engine systems we have. There are so many unknowns with how our bodies work, and even with just the heart itself, there’s so much more to explore.”
-Hamid Sadat, assistant professor of mechanical engineering
“Some previous studies have surmised that all the leaflets are similarly calcified, but that’s not accurate,” Sadat says. “Through our advanced simulations, we’ve realized that the calcification pattern is strongly influenced by leaflet dynamics, aortic hemodynamics and biotransport, leading to non-uniform and distinct calcification across the leaflets. We’ve found that it’s only certain parts of the leaflets that become stiff, usually the middle or base of the valve.”
Before taking on this project, Sadat had never used his fluid dynamics expertise to study a medical problem. Now, he plans to tackle even more in the health care field.
“It’s really interesting how complex these systems are in the body when compared to the best engine systems we have,” Sadat says. “There are so many unknowns with how our bodies work, and even with just the heart itself, there’s so much more to explore.”